It's not just about having "foot pain" or "hand numbness"—the exact distribution of your symptoms creates a precise map that guides every treatment decision. Where you feel burning versus tingling, which fingers go numb, and even what time of day symptoms worsen all provide crucial clues that shape your path to finding a diagnosis, recommending a possible treatment, and ultimately leading to recovery.
What Nerve Pain Location Means for Treatment
Where Do You Hurt?
We understand the burden that chronic pain has on you and those closest to you and offer treatment options to reduce or eliminate your pain.
Information is key to ridding yourself of chronic pain for good. Our library articles explore common complications of major surgery, including sexual dysfunction after groin surgery, foot drop after a knee replacement, post-surgical groin due to hernia or C-section, and causes of chronic regional pain syndromes.
 Learn More
Learn More
FAQs About Pain Location
 These frequently asked questions address the concerns that peripheral nerve surgeon Dr. Eric H. Williams often hears patients express most about how their specific pain patterns influence treatment options and surgical outcomes.
These frequently asked questions address the concerns that peripheral nerve surgeon Dr. Eric H. Williams often hears patients express most about how their specific pain patterns influence treatment options and surgical outcomes.
Understanding the relationship between your specific symptoms and the nerves involved is a crucial part of creating an effective treatment plan. Dr. Williams takes the time to carefully evaluate each case, using his extensive training and experience to tailor surgical approaches that offer the greatest chance of long-term pain relief and restored function.
If you don’t see your specific question listed or would like to discuss your situation in more detail, Dr. Williams will be happy to answer any additional questions during your consultation. Your comfort, clarity, and confidence in the process are his top priorities.
Does the Exact Location of My Pain Really Matter for Treatment?
Each peripheral nerve supplies sensation and function to specific areas of your body, much like electrical circuits in your home serve particular rooms. When you describe burning pain on the top of your foot versus the bottom, you're telling Dr. Williams which nerve system needs attention.
This specificity matters because different nerves require different surgical approaches, even when they're located near each other. For example, the peroneal nerve controls sensation on the top of your foot, while the tibial nerve handles the bottom. These nerves can be compressed at different locations and require completely different surgical techniques for effective treatment.
The distribution of your symptoms also reveals whether you're dealing with a single nerve problem or multiple nerves. Patients with conditions like diabetes often develop nerve compressions in several locations simultaneously. Each affected nerve requires individual attention for optimal results.
I Have Pain in Multiple Areas. Does This Mean I Have Multiple Problems That Need Separate Treatments?
A single nerve can cause symptoms in multiple locations along its course. The ulnar nerve, for instance, can create numbness in your ring and little fingers while also causing pain at your elbow where it becomes compressed. In this case, treating the compression at the elbow addresses all the related symptoms.
However, some patients do have multiple nerve compressions, particularly those with diabetes or inflammatory conditions. High blood sugar levels cause nerve swelling throughout the body, potentially leading to a compression wherever nerves pass through tight anatomical spaces. Each compression site may require its own surgical treatment.
Dr. Williams uses diagnostic techniques like nerve blocks to determine whether multiple pain areas are related or represent separate problems. If you have multiple nerve compressions or nerve injuries, he will try to develop a comprehensive treatment plan that may involve staging surgeries over several months or addressing multiple areas during a single procedure, depending on your specific situation. Also, it is important to remember that not every patient is a surgical candidate. If the area of pain is too large, there may be other treatments that are more likely to be helpful than peripheral nerve surgery. There may be times when medication management or electrical stimulation with a pain management team may be a serious consideration and the best option.
My Pain Seems to Move Around or Change Locations. Does This Mean Nerve Surgery Won't Help?
Pain that seems to move or change locations doesn't necessarily mean you're not a candidate for nerve surgery, but it does require careful evaluation to understand what's causing these variable symptoms. Several scenarios can create this pattern, and Dr. Williams will work to identify the underlying cause. Typically, the “wires” or nerves do not move. So pain that moves around to many areas does not neatly fit the template for a few or a single peripheral nerve, making surgery to target one nerve or a few nerves much less likely to help.
Some patients have multiple nerve compressions that become symptomatic at different times. As one area improves or worsens, you may become more aware of symptoms in other locations. This doesn't represent treatment failure but rather reveals the presence of multiple problems that may require individual attention.
Nerve pain can also radiate along the nerve's course, creating symptoms that seem to move from one area to another. The sciatic nerve, for example, can cause pain that travels from the buttock down the back of the leg to the foot. Understanding the nerve's anatomy helps Dr. Williams determine whether symptoms in different locations represent a single problem or multiple issues.
Some patients notice that treating one nerve compression reveals symptoms in other areas that were previously masked by more severe pain. This discovery is actually positive because it means the most problematic nerve has been successfully treated, allowing recognition of other issues that can now be addressed.
I've Had These Symptoms for Years. Does the Duration Affect Whether Surgery Will Help?
The duration of your symptoms does influence treatment planning and outcome expectations, but it doesn't automatically disqualify you from surgical treatment. Dr. Williams considers symptom duration alongside other factors to determine if you’re a good candidate for surgical treatment and set realistic expectations for recovery.
Longer symptom duration often indicates more established nerve damage, which can affect recovery speed and completeness. Nerves that have been compressed for years may take longer to recover after surgical decompression compared to recently compressed nerves. However, many patients with long-standing symptoms still achieve significant improvement with appropriate treatment.
The key factor isn't just duration but also symptom progression. Patients whose symptoms have remained stable or improved at times may have better surgical outcomes than those experiencing steady worsening. Dr. Williams evaluates whether your symptoms suggest ongoing compression or injury that surgery can address or irreversible nerve damage that might not improve significantly.
Some patients notice that their symptoms have changed character over time. Early nerve compression often causes intermittent tingling or numbness, while established compression may create constant numbness or burning pain. These changes help Dr. Williams understand the degree of nerve damage and predict surgical outcomes.
I Have Different Types of Sensations in the Same Area—Burning, Tingling, and Numbness. What Does This Combination Mean for Treatment?
The combination of different sensation types in the same area provides valuable information about the degree of nerve damage and helps Dr. Williams predict surgical outcomes. Different types of abnormal sensations indicate various aspects of nerve dysfunction associated with peripheral nerve pain.
- Tingling sensations often represent nerve irritation rather than severe damage. These symptoms may improve relatively quickly after surgical decompression because the underlying nerve function remains largely intact.
- Burning pain typically indicates more significant nerve dysfunction and inflammation. This type of pain often requires longer recovery periods after surgical treatment, but many patients still achieve substantial improvement. The intensity and constant nature of burning pain may require additional pain management strategies during the recovery period.
- Numbness represents loss of normal nerve function and can be more challenging to reverse completely. However, even partial improvement in numbness can significantly enhance function and quality of life. Some patients notice that protective sensation returns even if fine discriminatory touch doesn't fully recover.
The combination of all three sensation types suggests a nerve that's experiencing multiple types of dysfunction simultaneously. While this indicates more significant nerve problems, surgical decompression can still provide meaningful improvement by relieving ongoing compression and preventing further deterioration.
My Pain Feels Different in Different Locations. Does Each Area Need a Different Treatment Approach?
Different pain characteristics in various locations often indicate involvement of different nerves, each requiring specific treatment approaches. Dr. Williams maps both the location and character of your symptoms to identify all affected nerves and develop comprehensive treatment plans.
- Sharp, shooting pain typically follows nerve pathways and suggests nerve irritation or compression. This type of pain often responds well to surgical treatment because it indicates that the nerve retains function but is being mechanically compressed. Patients with predominantly shooting pain may see dramatic improvement after surgery.
- Deep, aching pain can indicate nerve compression at deeper anatomical levels or involvement of nerves that supply muscles rather than just skin sensation. These nerves may require different surgical approaches and often take longer to recover after decompression because they control more functions than purely sensory nerves.
- Surface burning or hypersensitivity suggests involvement of cutaneous sensory nerves that supply skin sensation. These symptoms can be particularly bothersome because normal stimuli like clothing or light touch become painful. Surgical treatment often provides good relief for these symptoms, though recovery may occur gradually over several months.
- Cramping or muscle weakness may indicate involvement of motor nerves that control muscle function. These symptoms require urgent attention because prolonged compression can lead to permanent muscle damage even paralysis. Early surgical intervention provides the best chance for recovery of motor function.
Dr. Williams considers the character of symptoms in each location when planning surgical procedures. Some areas may require nerve decompression, while others might need nerve repair or reconstruction. Understanding the different types of dysfunction helps prioritize treatment and set appropriate expectations for recovery in each area.
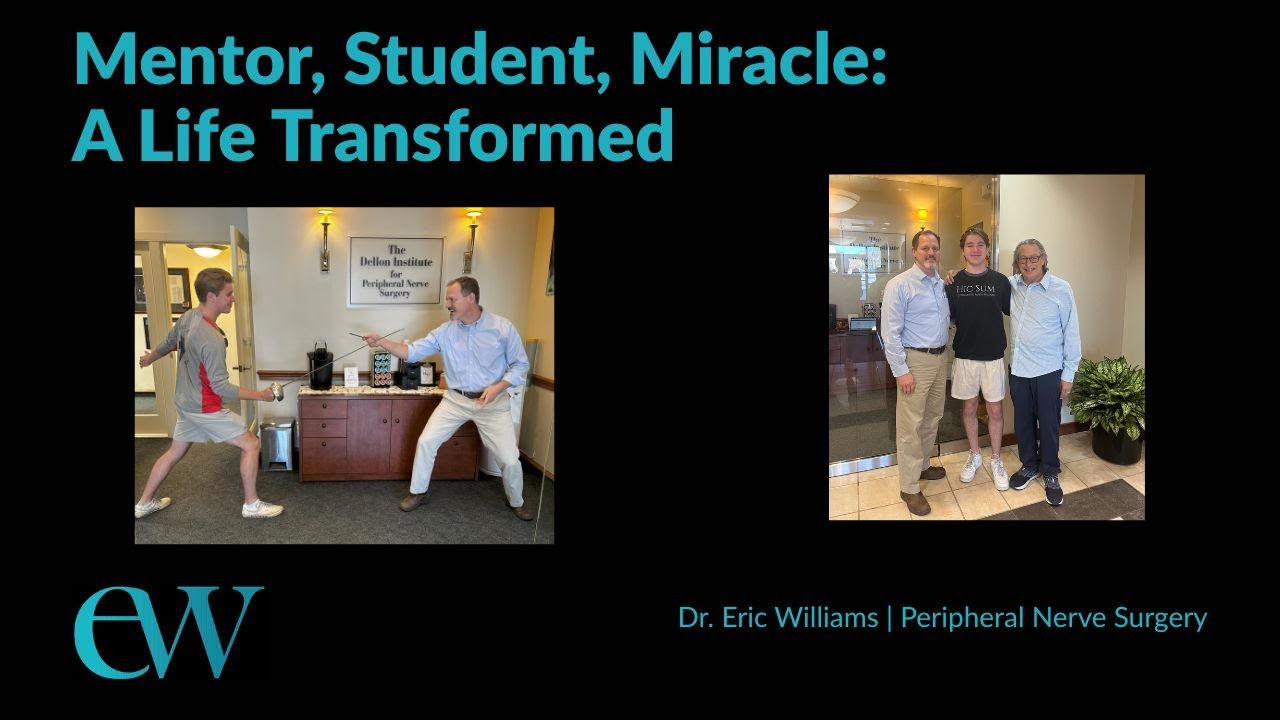
Patient Success Stories
Mentor, Student, Miracle: Innovative Nerve Surgery Ends Alex's Agonhy
Discover how a groundbreaking nerve surgery transformed Alex’s life after years of debilitating leg pain and misdiagnoses.
You Don't Have to Live With Pain Any Longer
Your journey to a pain-free future may include a visit to Dr. Eric H. Williams, MD, with The Dellon Institute for Peripheral Nerve Surgery. If you would like more information or want to request an appointment, simply call our office at (410) 709-3868 or fill out a contact form here.